
It excels in the insurance industry, providing medical facilities, education, and benefits to people working in the healthcare industry. STAR Medicaid coverage for low-income children was introduced in 1997 by the Harris Health System, one of our region’s public university health systems. The TAHP Credentialing Verification Organization (CVO) is responsible for receiving completed applications, attestations, and primary source verification documents for Medicaid-managed health plans. Community Health Choice Marketplace must review and approve all providers’ credentials at least once every three years.
Or
In 2018, Community Health Choice Marketplace enrolled 32 beneficiaries as the first group in CareerReady. CareerReady awards fellows with a scholarship to attend Houston Community Health Choice College to pursue a professional certification program. These programs include nursing, electrocardiogram technology, phlebotomy, paralegal, plumber, and office staff.
Registration Procedure For Community Health
For more benefits of medicare plans available on the Community Health Choice website, registration is compulsory. Registration steps are as follows:
Community Health Choice Providers: The Community Health Choice provider enrollment steps are listed below:
- Visit the Community Health Choices website.
- Click on “For Providers” at the top of the site.
- Click “Become a Community Provider” after clicking the “For Providers” option. Please complete the appropriate profile form on the website by clicking “Become a Community Provider” and submit it by mail/email/phone to apply to participate in Community Programs.
- Click Register Now.
- A Community Health Choice portal is open. In this portal, enter your tax number on the pages of the secure access application after clicking on “Register Now.” After that, click “Submit” to successfully register on the Community Health Provider Portal.
Guide To Community Health Choice Login
After registering for Community Health Choice, the next step is to log in to the Community Health Choice Login Portal. You can choose which of the two languages(English and Spanish) suits you for the Community Health Choice login. The registration steps are as follows:
Login At Community Health Choice Provider Portal: The steps for Login at Community Health Choice Provider Portal are as follows:
- Visit the Community Health Choices website.
- Click on the “For Providers” option. After that, a community health choice provider portal will appear.
- On the Community Health Choice Provider Portal website, click Become a Community Provider.
- Click register today.
- A secure access application page opens. Below the word “Secure Access Application” is a line “Click here if you are an existing user and want to reset your password.”
- In this line, click on the word “here,” which links to the sequence listed in the previous point.
- A Community Health Choice provider portal page opens. On this page, click Sign In.
- A Community Health Choice provider login page opens. Enter your username and password, then click “Log In.”
- You can tick mark “Remember Me” (optional) if you want to log into the Community Health Choice provider login portal in the future.
Requirements For Community Health Choice Login:
- Personal Computers, Laptops, Smartphones, Tablets, and Ipads.
- Community Health Choice Login website(www.communityhealthchoice.org).
- Good Internet Connectivity.
- Mozilla Firefox, Google Chrome, Microsoft Internet Explorer.
- Username and Password.
Reset Your Username And Password For The Portal
Many Community Health Choice insurance account holders forget their username or password during the Community Health Choice login period. For this solution to the issue, we have listed the following steps to reset your Community Health Choice login information:
Reset Steps For Community Health Choice Provider Login: The steps to reset your username or password on the Community Health Providers of Choice Portal are listed below:
- Visit www.communityhealthchoice.org.
- Click on “For providers.” A portal page for Community Health Choice providers opens.
- Click “Become a Community Provider” on this portal. Click Register Now.
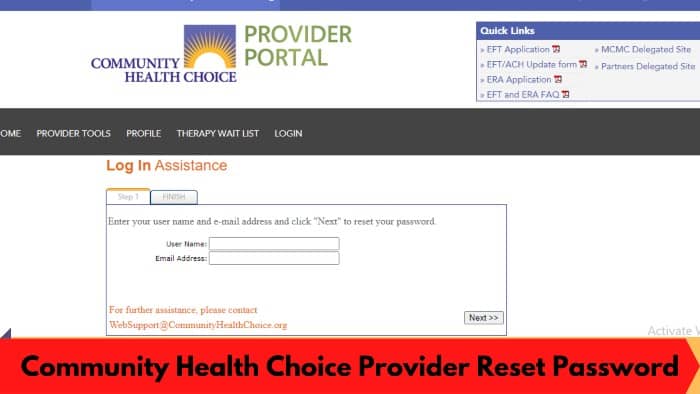
- Click on the Login menu on the Community Health Choice Providers portal. Click “Need help signing up?” in the provider’s login portal.
- Click Next to reset your password after entering your username and email address.
Eligibility For Community Health Choice Insurance
To participate in the Community Health Choice (HMO D-SNP), a member must:
- Eligible for Medicare Part A
- Registered with Medicare Part B
- Live in our service area
- Texas Medicaid Eligible Categories: QMB or QMB Plus.
As a dual beneficiary, the beneficiary’s benefits are paid first by Medicare and Medicaid. Medicaid coverage varies based on income, resources, and other factors. Benefits may include full Medicaid benefits and complete or partial payment of the member’s Medicare copayments (premiums, deductibles, coinsurance, or copayments).
How To Verify Eligibility?
- To check eligibility:
– Receive via the supplier portal
– Call operator services
- All members receive an identity card from the community
- All members must select a PCP or the community will assign one.
What Kind Of Services Are Covered?
Services covered by Community Health Choice (HMO D-SNP):
Covered Services
- Inpatient and Outpatient hospital
- Emergency Care
- Emergency
- Medical Service
- Laboratory
- Bone Scan
- Behavioral Health Services
- Drugstore
Additional Services/Value Added Services
- Dental
- Vision
- Transport
- Catering Service
- Over-The-Counter (OTC) Allowance
Provider Responsibilities:
- Check membership eligibility.
- Inform the community and other appropriate entities.
- Provide at least 90 days of written notice of termination, retirement, or relocation to the community outside the service area.
- A member has the right to make decisions about their care if they cannot make those decisions when necessary.
- A Member has the right to make decisions about their treatment in the event that the Member is not able to make those decisions at the time they are needed.
Methods For Payment Of Premium
The community has partnered with Change Healthcare and ECHO Health, Inc. for Electronic payment and invoicing. We describe it below Payment options and all the promotional items your office needs:
- Virtual Card Services: Virtual cards enable your office to accept payments such as credit card transactions and are typically received 7-10 days before paper checks as there is no delay in printing or sending. Your office will receive fax notifications containing a virtual card with a unique number for that payment transaction, your statement of payment (EOP), and a processing instructions page. Once you receive the virtual card number, enter the code into your agency’s credit card terminal to process the payment.
- EFT/ACH – Setting up an electronic funds transfer (EFT) is a fast and reliable method of receiving payments. If you want to sign up for EFT, you have two options:
-
- To register to receive EFT through the Settlement Advocate for Community Health Choice only, visit https://view.echohealthinc.com/EFTERADirect/CommunityHealthChoice/index.html.
- Visit https://view.echohealthinc.com/EFTERA/efterainvitation.aspx to sign up to receive EFT from all payers who process payments on the Settlement Advocated platform.
Plans Available At www.communityhealthchoice.org
Texas STAR Plan (Medicaid): The Community Health Choice Medicaid offers Medicaid for children and pregnant women. These programs are free for US residents who cannot afford health insurance. The Community Health Choice Medicaid follows the government provider’s pharmaceutical formula for Medicaid and CHIP. You can check the list at https://www.txvendrug.com/formulary/formulary-search.
This list will tell you:
- If the drug is in the prescription
- If the medication requires prior authorization
- If the medication you need is not your preferred medication, you must request an exception by calling Member Services toll-free at 1.888.760.2600.
Community Health Choice Marketplace: You may be eligible to purchase a Community Health Choice Marketplace coverage plan during the Special Enrollment Period (SEP) outside of the annual Open Enrollment Period (OEP). You must have experienced an eligible life event within the last 60 days to be eligible for Community Health Choice Marketplace
Benefits Of Registering With CHC Portal
The Community is always working for you and your family, from the benefits and special programs we offer to how our Member Services team can help you get the most out of them. Community Health Choice Medicaid benefits are listed below:
Top Doctors And Hospitals
They have a robust provider network and the largest hospital network in Southeast Texas. That is yet another reason to choose a plan near you.
Free 24-Hour Access To Telemedicine Services
Several community plans offer telemedicine services that allow you to talk to a certified physician for free via your phone, computer, or mobile device at any time of the day or night.
Manage Complex And Chronic Care Conditions
Based in Houston, Community Health Choice (Community) helps its members care for themselves and their families more effectively and informedly, including those diagnosed with chronic illnesses.
Beneficiary Protections
Medicare Advantage Organizations (MAOs) are responsible for ensuring that your organization and its Contract hospitals and critical access hospitals (CAH) apply the provisions of the Notice of Observation, Treatment, and Effects on the Nursing Eligibility Act or NOTICE in a straight line. All AAMs and other Part C vendors and suppliers, including pharmacies, must refrain from Medicare cost-sharing charges for covered individuals.
| Official Site | Community Health Choice |
|---|---|
| Portal Type | Login |
| Country | United States Of America |
| Services | Health Insurance |
| Managed By | Community Health Choice Texas, Inc. |
Customer Service Centers
Customer Service Centers are available through Community Health Choice Insurance for CHIP/CHIP Perinatal, Marketplace, STAR (Medicaid), and Medicare D-SNP members. Marketplace members can reach customer service representatives between 8:00 am to 5:00 pm Monday through Friday for Marketplace members, 8:00 am to 6:00 pm to 6:00 pm (Monday to Friday) Friday) 8:00 am to 8:00 pm (7 days a week, October 1 to March 31, and Monday to Friday, April 1 to September 30) at the Community Health Choice phone number.
Below are Community Health Choice phone numbers for various plans:
- Services for CHIP Members: Local no: 713.295.2294 and Toll-Free: 1.888.760.2600
- For Marketplace members: Local no: 713.295.6704 and toll-free 1.855.315.5386
- Benefits for STAR Members (Medicaid) – Local no: 713.295.2294 and Toll-Free: 1.888.760.2600
- For Medicare D-SNP members: Local no: 713.295.5007 and toll-free 1.833.276.8306
About Community Health Choice
The Community HealthChoices (CHC) program offers seniors and adults with disabilities physical health benefits, long-term services, and qualified support. The Pennsylvania State Health Care Corporation Medicaid program provides various benefits and services through its accredited managed care organizations. Keystone First Community Health Choice Medicaid, UPMC, and PA Health and Wellness are among them.
They provide affordable, coordinated, high-quality health care services. As one of the most extensive health plans in the Gulf Coast region, CHC is based in Houston and offers Children’s Medicaid (STAR) and CHIP. Their insurance and Medicaid plans cover over 400,000 people through a network of 9,000 doctors and 70 hospitals.
Frequently Asked Questions
Would You Like Assistance Finding A Service Provider Or Making An Appointment?
Call on Community Health Choice Phone Number!
Monday to Friday (except nationally recognized holidays) – 8:00 am – 5:00 pm – 6:00 pm
Local : 713.295.2294 – Toll free: 1.888.760.2600 – TTY: 7-1-1
How Can I Refer And Find Experts In Your Scheme?
We don’t need a reference to refer a member to a network expert. You can confirm a network specialist by visiting this website or calling Provider Services at 713.295.6704
How Do I Replace My Membership Card?
Print a temporary My Member Account ID card at CommunityHealthChoice.org > Member Login. Member Services will send you a permanent one. Or call toll-free at 1.888.760.2600.
Do I Have Access To Off-Network Services?
We provide members with medically necessary off-network and covered services unavailable on our network. When these services are available, members must use one of our network providers.
Conclusion
Community Health Choice Medicaid deals with health insurance plans for residents of the United States of America. We aim to provide quality care to everyone to live long and healthy lives. Your team members are trustworthy and caring people who work alongside our community members, vendors, and partners.
They work hard to improve the health and well-being of underprivileged Texans, opening the door to health care and health-related social services. In this case, you can view Community Health Choice Medicaid Providers List by clicking the Find a Doctor menu on their website.